Abstract
Introduction: Hodgkin's lymphomas (HL) is a highly curable lymphoid neoplasm historically treated with the ABVD regimen (Doxorubicin, Bleomycin, Vinblastine, Dacarbazine), with an acceptable toxicity profile. HL has a unique bimodal distribution with a peak incidence in adolescent/young adults. The 5-year relative survival rate is ~ 90%, however; 30-40% of patients relapse within first two years and require salvage treatment. Globally, few studies have assessed the predictors of adverse outcomes in HL. This analysis focuses on the association of various sociodemographic/socio-economic determinants on HL mortality.
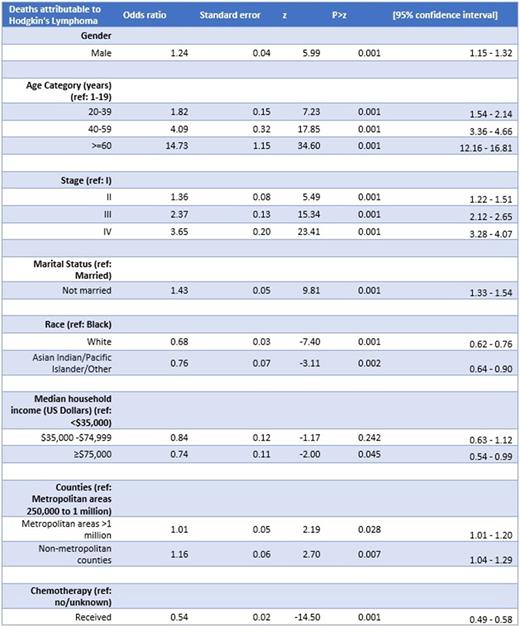
Methods: This cross-sectional study evaluated patients aged 1 to ≥85 years diagnosed between 2000-2019 with HL utilizing 17 US registries in the Surveillance, Epidemiology and End Results (SEER plus) database. The SEER program has been developed by the National Cancer Institute, and provides information on cancer statistics across geographically diverse US regions. The primary outcome was cancer-specific mortality. Differences in outcomes were estimated by univariate logistic regression. Variables significant on univariate analysis were entered into multivariable logistic regression models. Complete case analysis approach was used. Coefficients are reported as odds-ratios (95% confidence intervals). P-value <0.01 was considered significant given multiple comparisons. Analysis was conducted using Stata/BE version (Statacorp LLC, College Station, TX).
Results: A total of 43,185 [n=19,365 (45%) female] HL patients were included between 2000-2019. Age groups were represented as 12% 1-19 years (y), 39% 20-39 y, 25% 40-59 y, 23% ≥60 y. Of these, 32,518 had a documented Ann Arbor Stage (18% Stage I, 41% Stage II, 21% Stage III, 20% Stage IV). Data on B-symptoms was available from 2010 onward, with 45% reporting ≥1 B-symptoms. Chemotherapy was administered in 81% of patients.
Racial demographics included Whites (82%), Blacks (11%), and Asian Indian/Pacific Islander/Other (AI/PI/O) (7%). Median household income (MHI) (inflation-adjusted to 2019) were grouped into those earning <$35,000 (1%), >$35,000- $75,000 (66%) and >75,000(33%). Geographic distribution was as follows: metropolitan areas (population >1 million) 60%, metropolitan areas with population 250,000 to 1 million (21%), and non-metropolitan counties (18%). 47.8% of the adult HL patients were married.
Mortality attributed to HL was reported in 6,261 (14.5%). Multivariable analysis revealed a higher mortality in males [Adjusted odds ratio (aOR), 1.24; 95% confidence interval (CI) 1.15 - 1.32] compared to women. Age ≥60 at time of diagnosis had higher mortality (aOR 14.73; 95% CI 12.16 - 16.81) among all age groups. Mortality was highest in those with Stage IV disease (aOR 3.65; 95% CI 3.28 - 4.07) compared to Stage I disease. Chemotherapy administration was associated with lower odds of death (aOR 0.54; 95% CI 0.49 - 0.58) compared to not receiving chemotherapy.
Among the socio-economic determinants of health, white race (aOR 0.68; 95% CI 0.62 - 0.76) and AP/PI/O races (aOR 0.76; 95% CI 0.64 - 0.90) had significantly lower mortality when compared to Blacks. Unmarried patients had a higher mortality (aOR 1.43; 95% CI 1.33 - 1.54) than married patients. Patients with higher strata of MHI had significantly lower mortality than lower MHI (75K versus <35K aOR= 0.74; 95%CI= 0.54-0.99). Those living in heavily populated metropolitan areas >1 million (aOR 1.10; 95% CI 1.01 - 1.02) or non-metropolitan/smaller counties (aOR 1.16; 95% 1.04 - 1.29) were associated with a higher mortality than average populated metropolitan areas of 250,000 to 1 million. These associations between sociodemographic factors and HL-specific mortality remained statistically significant on risk adjusted and subgroup analyses.
Conclusions: This study underscores the significant influence of sociodemographic/socioeconomic factors on mortality in patients with HL after adjustment for various clinical predictors. Patients that are black, not married, or with lower household income had higher rates of mortality. Those living in heavily populated or in remote non-metropolitan areas/smaller counties fared worse in terms of death compared to averagely populated metropolitan areas. These findings need to be validated in prospectively designed studies assessing modifiable and non-modifiable predictors of adverse outcomes in HL patients.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal